
NEWSLETTER
February 2024

Welcome to the Maina Foundation Newsletter!
An Inspiring Interview With Liz K, a Patient With Metastatic Cancer
By Manju Soni
Dear friends,
This month’s newsletter is an interview with my old neighbor and very good friend, Liz K, who, at the age of 63, was diagnosed with metastatic endometrial (uterine) cancer. After a turbulent course of treatment, Liz has made the difficult decision to stop treatment.
Thank you, Liz, for sharing your experience with me and our readers.
Please tell us a bit about your diagnosis.
Thank you, Manju.
My diagnosis of endometrial cancer came in December, 2022.
I had been very active with volunteer work during 2022 and felt great. The only thing I noticed was occasional blood on my panties. Since I did not have many risk factors for endometrial cancer, I delayed making an appointment with an OBGYN. Finally, in November, 2022, after confiding in my husband, he pushed my primary care doctor to get me in to see an OBGYN immediately. The OBGYN performed a very painful biopsy with no type of local anesthetic. Despite my inability to take the pain, there was enough tissue to determine characteristics of the cancer cells. After that visit, I had an ultrasound and CT scan to determine how far the cancer had advanced. The cancer had spread to my fallopian tubes, ovaries, upper femur, and liver.
What was your initial reaction to the news of your illness?
I was shocked that it was so advanced. I had had no pain or other symptoms,
I felt well, no weight loss and I was very active. I felt good. I had
occasional bleeding, but ignored it for a while because I was so busy. By
the time I had the investigation it had metastasized.
My husband has been a pillar of strength. He’s a scientist, and used to work for Pfizer. He took charge. I was sure I’d get through it and I’d be okay with treatment.
What has your journey been since then?
The first approved line of treatment for this cancer were the combined
chemo drugs, Carboplatin and Paclitaxel. I started them in January 2023. As
expected, they made me lose my hair, but I also developed ascites (fluid
accumulation) in my tummy, which affected my breathing.
They also proved ineffective as my cancer kept growing, so after three months, the first regimen was stopped and the doctors began a second regimen on me.
I was switched to a combination of Keytruda (infusion every 3 weeks) and Lenvima (daily pill). There were many side effects with these drugs that had to be monitored closely. I developed neck pain, mainly at night. My neck would be so painful it was difficult to even turn in bed. My blood pressure went up and my thyroid stopped functioning, a condition called hypothyroidism.
The tumors appeared to be going down, but in July, I was admitted again because of memory problems. My husband noticed I was asking weird questions, or I’d go into the study and be there for hours, not knowing how to organize things. My executive functions were quite poor.
I was admitted to the hospital to see if the cancer had spread to my brain. After many tests and scans, they determined that there was no spread to the brain. Nevertheless, I had no appetite and was losing lots of weight while on the drugs. My memory was so bad, we decided to stop the chemo drugs.
They were restarted again later, but my urine protein went up, and my confusion was worse again, another sign to the doctors that I had to stop the drugs.
My oncologist stopped everything and prescribed high dose prednisone to see if brain inflammation was causing the problems.
I was very depressed at this stage.
The prednisone was eventually tapered to 10mg. My appetite came back and my blood pressure was under control. I responded well to the prednisone and they concluded there must have been some swelling in my brain.
After that, my husband and I made the difficult decision, with my oncologist's approval, to stop active treatment and to enroll in hospice, where I am currently.
Do you have a family history of cancer?
None in my immediate family. My dad’s sister had colon cancer.
Would you have done anything differently?
I’m not sure really. I was under an insurance plan that meant I had to go
to a specific hospital. The oncologist there seemed so rattled by my
diagnosis, she’d pull out a calendar and be confused when the next
treatment would be. My husband and I didn’t feel confident I’d get the best
care there.
I changed my insurance and saw someone at Duke Oncology. I felt much more comfortable. I suppose what I learned was you need to have confidence in your healthcare team.
Cancer is said to be expensive; can you elaborate?
The cost is huge. For example, the cost of one month of Lenvima tablets was
over $21K. I hit my deductible pretty quickly. But after that the insurance
paid for most things. It made me wonder how devastating it would be if you
don’t have good insurance.
I recently read When Breath Becomes Air by Dr. Paul Kalanithi, a neurosurgeon, who died of lung cancer. And when he first learns of his diagnosis he says, “And with that, the future I had imagined, the one just about to be realized, the culmination of decades of striving, evaporated.”
How has your perspective changed since learning about your illness?
It’s been an emotional rollercoaster. Every day has its ups and downs. The
hospital referred me to a social worker, but my experience with them wasn’t
very helpful.
I had to reset my expectations after each hurdle or change in my treatment. I had to adapt every time. At the moment it’s harder, there are no scans to monitor progress or deterioration in my tumor. I’m feeling good, but my energy level is going down at present.
The hardest time for me is now, the waiting. Not knowing how long I’m going to last.
What has been the most challenging aspect of your illness?
The uncertainty is difficult to deal with.
The side effects of the drugs are another issue. Simple side effects can have a huge impact on one’s life. People who prescribe these drugs should warn patients of them.
The neck pain was very distressing. I tried different pillows, and arthritis rubbing meds, nothing helped. It was clearly related to the drugs because it stopped when I stopped treatment.
I also had constipation while on chemo. I had to take constipation pills a few times a day. They would give me diarrhea and that was harrowing. Now it’s different, less diarrhea and I try to eat more fiber with lots pf water. I drink about 6-7 glasses of liquid a day and stay away from caffeine.
Are there any particular moments or experiences that have brought you
comfort or joy, or made you laugh?
Our cat, Krauss, was a wonderful companion. Sadly, he was quite elderly and
had kidney failure, and we had to put him down a few weeks ago. That was
very hard to deal with.
He was so much part of our family. He had certain habits, like watching TV with us. We had scattered heating pads around for him, and he would snuggle up on one on the sofa between us, purring as we petted him. I’d got into the habit of checking up on him frequently. I miss him a lot.
My biggest pleasures are walking, and getting out into sunshine. I try to walk every day, as much as I can manage, which varies from 1 – 4 miles. Recently, when we visited Savannah, Georgia, I walked up to 5 miles per day.
I enjoy reading books. At the moment I’m reading Violeta: A Novel by Isabel Allende. I’m still with my book group, it’s an in-person group, and they’ve been very supportive.
I enjoy watching shows on TV and listening to podcasts.
How do you navigate interactions about your illness with family and
friends?
My husband coped by digging into the research and focusing on
practicalities. It was his way of dealing with everything. He keeps busy
with exercise and disc golf.
We lean on each other and are both pretty frank about what’s happening, often resorting to a type of gallows humor. I feel like I can tell him anything and he would get it.
Our son, who is in his twenties, was of course very worried, and still is. He comes over once a week.
Do you have any advice for our readers who may be in a similar
situation?
Yes, surround yourself with things that make you happy. Don’t focus too
much on making others happy. You need to focus on your own emotional and
mental self-care.
What are you reading, listening to or watching currently?
Podcasts: I listen to The Daily by the New York Times, and Preet Bharara’s podcast, as well as NPR’s Fresh Air.
On TV we’ve been enjoying Oscar nominated movies, and on Hulu there’s a show called Feud that I quite liked. The first season was about the rivalry between Betty Davis and Joan Crawford. It gives you a lot of background to cinema during those days. The second season is about Truman Capote who wrote the true crime book, In Cold Blood. That season is about Capote and the rich women he befriended in high society in New York.
Is there anything else you would like to share or express about your
experience?
Depression is tough to deal with, you have to take it day by day.
Thank you, Liz, for talking to us about your brave journey!
And to our Maina Foundation newsletter readers, thank you for reading and your valuable support!
Manju Soni (she/her) (pen name: M. J. Soni) is a former eye surgeon turned author. She is the author of Defying Apartheid, her debut nonfiction book that captures her experiences of being a young activist against apartheid. Her short fiction and essays has appeared in Ellery Queen Mystery Magazine, Akashic Books, Apeiron Review and The Establishment. She’s a member of Crime Writers of Color and Sisters in Crime (National and Connecticut.
News!
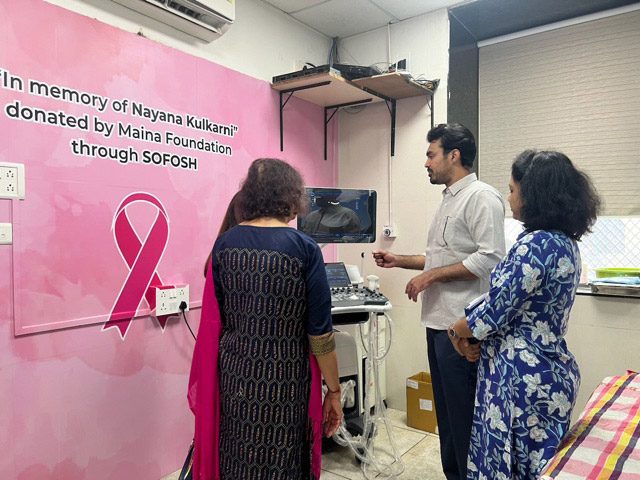
In early February 2024, Maina Foundation founder, Alka Shrikhande, visited Sassoon Hospital in Pune, where she met Dr. Ansari, the Director of Oncology, who explained to Alka the workings of the ultrasound machine bought with funds donated by Maina Foundation.
The machine was donated in memory of Nayana Kulkarni, a successful lawyer in New York City, and the daughter of Maina Foundation’s board member, Dr. Sujata (Jayashree) Kulkarni. She succumbed to breast cancer at the young age of 44.

We thank you for your continued support!
For more information on Maina Foundation, and to help its mission, go to https://mainafoundation.org or contact us at 860-434-3985 or info@mainafoundation.org
SAVE A LIFE - DONATE NOW
Donations can also be mailed to:
8 Peppermint Ridge, Old Lyme, CT 06371, USA
